PA Program Goals and Competencies
Program goals
University of Bridgeport’s PA Institute (PAI) has established the following five goals which support the mission and outcomes of the program. Each goal has defined benchmarks and associated data which demonstrate how they are being met. Benchmarks are identified in figures and graphs as a purple line.
Benchmarks
The program values diversity and aims to recruit a cohort with various backgrounds and experiences. We have identified specific student demographics which we actively recruit through outreach, increased student support, and engagement. Based on these values and efforts, the program has set a benchmark of 40% or greater of matriculated students in each cohort identifying themselves as one of the following: veteran, first generation college student, multilingual, from a family that lives in a health professions shortage area (HPSA) or medically underserved area (MUA), or DACA recipient.
Cohort 2026 fell just below benchmark in this category. This is the first cohort since the goal was established that fell below benchmark. The average for Cohorts 2023-2026 remains well above benchmark: overall, 48% of these students identified with at least one of the defined diverse backgrounds and experience categories. In response, the program will continue to increase outreach efforts for active recruitment.
FIGURE 1 Percentage of Students Identifying As Veteran, First Gen, Multilingual, HPSA, MUA, or DACA by Cohort

In 2021, UBPAI developed a program called “Bridge to Bridgeport” to increase recruitment through partnerships with historically marginalized communities, health professional shortage areas, and medically underserved areas. One of the events that took place in 2023 was a faculty-led “High School PA Day” in which forty local high school students interested in pursuing health careers came to the UB campus to learn more about the PA profession.
For this goal, the program has set a benchmark of organizing or participating in a minimum of five faculty-led outreach or recruitment events annually.
FIGURE 2 Number of Total Outreach Events by Year
| Year | Number of Events |
|---|---|
| 2021 | 7 |
| 2022 | 8 |
| 2023 | 13 |
| 2024 | 6* |
*Data current up to November 2024
The University of Bridgeport is a diverse institution of higher education, with students from across the United States and around the globe. The program has collaborated with leaders in the undergraduate biology and health sciences departments to develop an undergraduate Pre-PA Track curriculum. The undergraduate Pre-PA Track was first offered in Fall of 2022. Beginning with the 2023-24 cycle, the program has set a benchmark for a 100% increase in the number of qualified applicants from the University of Bridgeport over the next 5 years.
FIGURE 3 Percent Increase Of Eligible UB Graduate Applicants By Year Since 2023-24 Admissions Cycle

Benchmarks
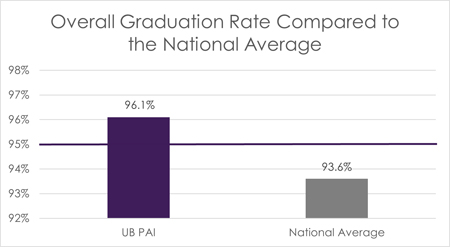
UB PAI takes pride in having a student-focused approach, aiming to increase student retention, and prepare graduates to be skilled and competent in the clinical field. Since inception, the program has an overall graduation rate of 96.25%. UBPAI graduation rates have been higher than the national average graduation rates (93.6%), according to national data from the 35th PAEA Annual Report. The program has set a benchmark of 95% overall graduation rate for the program.
FIGURE 4 Overall Graduation Rate Compared to the National Average
All students meet with their faculty advisor regularly throughout the program. The program recognizes the importance of this as an opportunity for mentorship, collaboration, and support. As part of the Exit Survey distributed to all graduates, students are asked to rate their satisfaction with faculty advisement during their time in the program. This item is scored on a 4-point Likert scale (1 – Highly Dissatisfied, 2 – Dissatisfied, 3 – Satisfied, 4 – Highly Satisfied), and the program has set a benchmark score of 3 to demonstrate that students are satisfied overall with faculty advisement in the program.
FIGURE 5 Graduates’ Satisfaction With Faculty Advisement (Cohort 2021-2024)

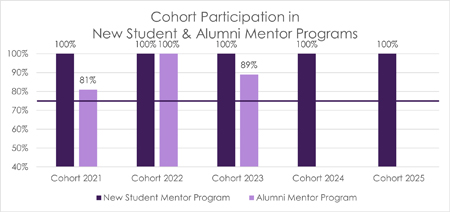
As part of UBPAI’s culture of support, students can work with a mentor in two available mentorship programs. As students prepare to matriculate into the program, they are offered the opportunity to connect with a peer mentor. This New Student Mentor Program allows incoming students a chance to ask questions, gather advice, and have a familiar face available as they start PA school. Similarly, as students are about to graduate, they can choose to participate in the Alumni Mentor Program where students are paired with an alumnus of PAI who is working in a field they are interested in, living in area where they plan to relocate, or has similar interests. These programs foster collaboration and support between peers. UBPAI has set a benchmark of 75% of the cohort participating as mentees in both programs.
FIGURE 6 Cohort Participation in New Student and Alumni Mentor Programs (Cohort 2022–2026)
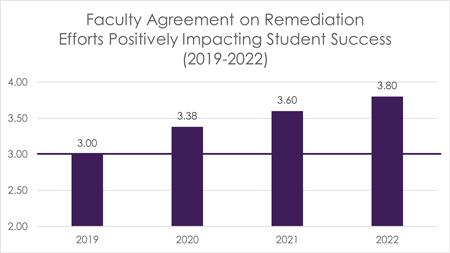
UBPAI continually strives to positively impact student success by identifying and addressing deficiencies in students’ knowledge, skills, or behavior during the program. An annual survey of faculty members asks faculty to evaluate the remediation processes’ effectiveness on improving student performance. This item is scored on a 4-point Likert scale (1 – Strongly Disagree, 2 – Disagree, 3 – Agree, 4 – Strongly Agree), with a benchmark score of 3 to demonstrate that faculty agree that the remediation efforts positively impact student success.
FIGURE 7 Faculty Agreement on Remediation Efforts Positively Impacting Student Success Effectiveness, 2019-2022
Benchmarks
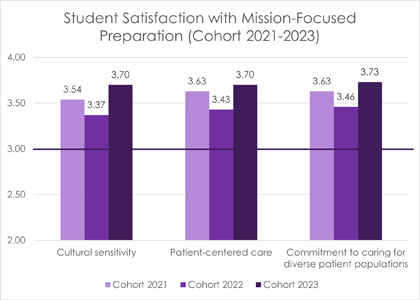
UBPAI values educating students with the knowledge and skills to prepare them to work with diverse patient populations, practicing culturally sensitive and patient-centered care. Data has been gathered related to graduates’ satisfaction with these specific mission-focused components. These items are scored on a 4-point Likert scale (1 – Highly Dissatisfied, 2 – Dissatisfied, 3 – Satisfied, 4 – Highly Satisfied), with a benchmark score of 3 to demonstrate that students are satisfied with the preparation provided in each of these categories.
Students were asked how satisfied they were with the program’s preparation
- to practice with cultural sensitivity
- to practice patient-centered care
- for commitment to caring for a diverse patient population
FIGURE 8 Student Satisfaction With Mission-Focused Preparation (Cohort 2021–2024)
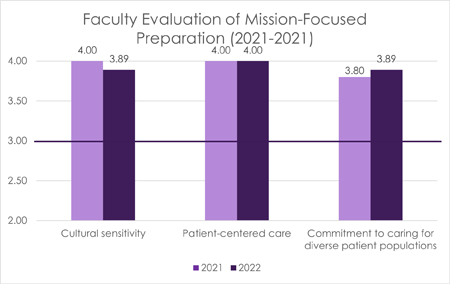
UBPAI analyzes the faculty’s impression of the curriculum-driven mission, including culturally sensitive and patient-centered care. This data was first collected in 2021 and is collected annually. These items are scored on a 4-point Likert scale (1 – Strongly Disagree, 2 – Disagree, 3 – Agree, 4 – Strongly Agree), with a benchmark score of 3 to demonstrate that faculty agree that curriculum is mission-focused on each of these categories.
Faculty members are asked to assess how well the PA curriculum prepares students for the following activities:
- Practice with cultural sensitivity
- Practice patient-centered care
- Commitment to caring for diverse patient populations
FIGURE 9 Faculty Evaluation of Mission-Focused Preparation (2021 - 2023)
Supporting the program’s commitment to diverse patient populations, MSPA 630 Special Populations Selective course was first offered for Cohort 2023. Specific data is collected regarding preceptor evaluation of the students’ ability to demonstrate cultural sensitivity and patient-centered care. These items are scored on a 5-point Likert scale (1 – Below Expectations, 2 – Approaches Expectations, 3 – Meets Expectations, 4 – Exceeds Expectations, 5 – Outstanding), with a benchmark score of 3.5 to demonstrate that preceptors agree that students are meeting expectations related to these abilities.
FIGURE 10 Average Preceptor Evaluation Score of Students’ Cultural Sensitivity (Cohort 2023 - 2024)

Benchmarks
UBPAI recognizes competence of medical knowledge through first-time PANCE pass rates. The program has set a benchmark of meeting or exceeding the national average for first-time PANCE pass rates. Of note, the program did not meet its goal in 2021 and implemented a focused PANCE preparation plan to address the deficiency. Since that time, all cohorts have achieved a 100% first-time PANCE pass rate.
FIGURE 11 Annual Pance Pass Rates for First-Time Test Takers Compared to National Average

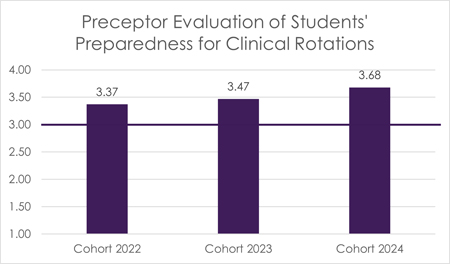
Annually, preceptors are surveyed on their impression of the preparedness of students entering the clinical phase. This is an aggregate impression of students’ preparedness provided by their didactic education in topics including medical interviewing, physical exam, oral case presentations, written documentation, knowledge of diagnostic studies, performing clinical procedures, and forming/implementing management plans. These items are scored on a 4-point Likert scale (1 – Not Prepared, 2 – Poorly Prepared, 3 – Prepared, 4 – Very Prepared), with a benchmark score of 3 on the average of all preparedness categories, demonstrating that more than half of the preceptors responded positively.
FIGURE 12 Preceptor Evaluation of Students’ Preparedness for Clinical Rotations
The UBPAI curriculum prepares students to manage acute, chronic, preventative, and emergent encounters in various health care settings across the lifetime. The program conducts continued analysis of the curriculum and monitoring of student scores on exams throughout the program, including on the PAEA End of Rotation (EOR) exams administered during the clinical year. The program has set a benchmark of mean EOR scores exceeding the national average for each exam.
FIGURE 13 End of Rotation Mean Scores Compared to National Averages (Cohort 2022)
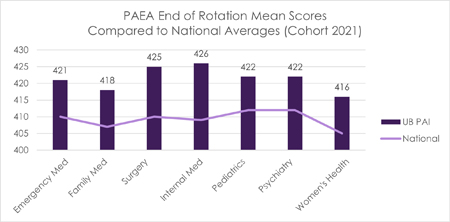
FIGURE 14 End of Rotation Mean Scores Compared to National Averages (Cohort 2023)

FIGURE 15 End of Rotation Mean Scores Compared to National Averages (Cohort 2024)

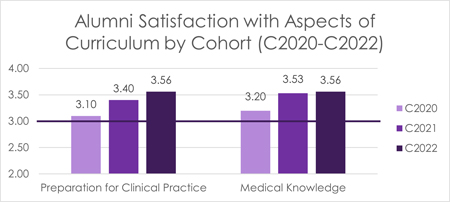
Alumni are asked to rate their satisfaction with their medical knowledge and their preparation for clinical practice. These items are scored on a 4-point Likert scale (1 – Highly Dissatisfied, 2 – Dissatisfied, 3 – Satisfied, 4 – Highly Satisfied), with a benchmark score of 3 to demonstrate that alumni are satisfied with the training received in both categories.
FIGURE 16 Alumni Satisfaction With Aspects of Curriculum (2020-2023)
Benchmarks
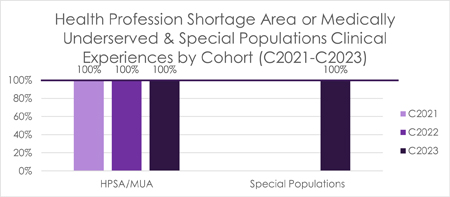
The program has a variety of clinical rotations which expose students to diverse communities and patients. In an effort for increased exposure to diverse communities, the program has set a benchmark of 100% of students completing at least one rotation in a HRSA-designated health profession shortage area or medically underserved area and one additional rotation focused on a special population. Special populations include but are not limited to, those who are underserved, underrepresented, at-risk or vulnerable. MSPA 630 Special Populations Selective course was first offered for the Cohort 2023.
FIGURE 17 Health Profession Shortage Area or Medically Underserved & Special Populations Clinical Experiences by Cohort (2021-2024)
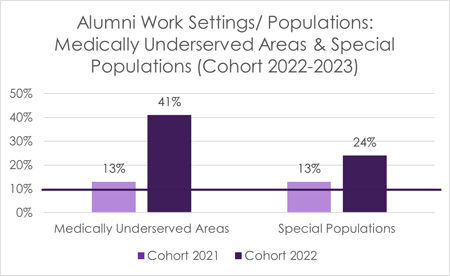
As part of the one-year alumni survey, data is collected related to alumni employment settings. As the Special Populations Selective was introduced, data was collected specific to alumni working with special populations and in medically underserved areas. The program has set a benchmark of 10% of alumni working in a HRSA-designated medically underserved area and 10% of alumni working with a special population at one-year post graduation. This data is based upon those students who respond to the one-year alumni survey sent out annually, with an average response rate of 49% for Cohorts 2021-2023.
FIGURE 18 Alumni Work Settings/ Populations: Medically Underserved Areas & Special Populations (Cohort 2021-2023)
Program competencies
Graduates of the University of Bridgeport Physician Assistant Institute will be able to demonstrate competence in the following areas:
- PO1: Elicit and interpret an accurate medical history from a patient. (PK)
- PO2: Perform an appropriate physical examination and accurately interpret findings. (PK)
- PO3: Utilize pertinent patient data and diagnostic interpretation to formulate a differential diagnosis. (PK)
- PO4: Demonstrate clinical reasoning and problem-solving skills to create a management plan. (PK)
- PO5: Accurately perform the technical skills utilized in care of the patient. (PK)
- PO6: Demonstrate effective communication skills necessary to work in healthcare teams. (HLC, ICP)
- PO7: Demonstrate culturally sensitive care with a patient-centered approach. (PK, HLC)
- PO8: Counsel and educate for disease prevention and promotion of healthy lifestyle. (PK, SPH, HLC)
- PO9: Understand the role of the PA and adhere to professional standards in healthcare settings. (ICP, PL, HCF)
- PO10: Identify the roles of various providers in the healthcare team including alternative or complementary practitioners. (HCF)
Definitions of the abbreviations are as follows: Patient-Centered Practice Knowledge (PK), Society and Population Health (SPH), Health Literacy and Communication (HLC), Interprofessional Collaborative Practice and Leadership (ICP), Professional and Legal Aspects of Health Care (PL) & Health Care Finances and Systems (HCF). Abbreviations are based on the Competencies for the Physician Assistant profession.
Together, let’s start something great.
Contact us today!
Request More Information- Phone1‑800‑392‑3582
- ApplicationApply Now
